Xenical Vs Other Weight Loss Medications
How Xenical Works and Who Benefits Most
Standing in the kitchen one night, a person imagines choosing a different path: this pill acts locally in the intestines to block dietary fat from being absorbed, so some calories simply pass through instead of being stored.
Clinically, it's most useful for adults with a BMI over 30 or over 27 with obesity-related conditions; it suits people who prefer a non‑central nervous system approach and those who want weight loss without stimulants. Many patients also find it complements lifestyle changes because it rewards lower-fat choices.
Side effects are usually gastrointestinal and can be managed with diet and a daily multivitamin; rare serious effects mean doctors screen for liver disease and pregnancy. With realistic expectations and guidance, patients can aquire sustainable habits and see modest yet meaningful results. Expect realistic timelines; typical loss is modest over months with sustained adherence required.
Comparing Side Effects: Xenical Versus Newer Options

Clinicians often frame side-effect profiles as the deciding factor when choosing therapy, and the contrast is striking. xenical works in the gut and causes oily stools, urgency, and sometimes flatulence, reflecting fat malabsorption; this can impact social life and adherence. Fat-soluble vitamin reduction means multivitamin monitoring is neccessary.
Newer agents like GLP-1 receptor agonists (eg, semaglutide) more commonly produce nausea, vomiting, constipation, and decreased appetite, with rare reports of pancreatitis or gallbladder disease. Naltrexone–bupropion brings different risks: insomnia, dry mouth, blood pressure elevation, and seizure risk in susceptible people. Side effects may be intense in the beginning but often lessen.
Choosing between them depends on comorbidities, tolerance, and lifestyle: some patients prefer avoiding injections, others prefer fewer social side effects despite metabolic monitoring. Shared decision-making and clear expectations reduce surprises and occassionally improve adherence. This context shapes realistic treatment expectations.
Weight Loss Efficacy: Trials, Numbers, and Expectations
In clinic many people ask what real results look like, and trials offer a measured story. Studies of orlistat (xenical) show modest but consistent additional loss versus placebo, so clinicians stress steady progress over dramatic change.
Pooled analyses suggest orlistat adds about three kilograms on average at one year compared with placebo and doubles the chance of losing at least five percent of body weight. Individual outcomes depend on diet, activity, and tolerability.
Set expectations: aiming for 5–10% loss over several months is realistic, and even modest reductions improve blood pressure and cholesterol. Discuss side effects and strategies to maintain adherence, because Occassionally gastrointestinal effects lead patients to stop treatment. Review goals regularly with provider.
Safety, Contraindications, and Long-term Health Considerations

I remember advising a patient about xenical, imagining both relief and apprehension as we reviewed medication interactions. We emphasized checking vitamin levels, liver tests, and personal history so early issues are spotted and managed collaboratively.
Contraindications were clear: pregnancy and chronic malabsorption syndromes exclude use, while caution is advised for patients with compromised liver function or on cyclosporine. Detailed history taking reduces risk and guides safer alternative selection and planning.
Over months, some patients experienced persistent oily stools and needed vitamin supplements; others benefited from weight maintenance. Regular follow-up tracks both efficacy and subtle metabolic changes that may Occassionally prompt adjustments reviewed with primary care.
Decisions about continuing treatment depend on individual risk profiles, lifestyle changes, and long-term goals. Clinicians should discuss rare hepatic events, supplement strategies, and realistic expectations so patients can make informed, choices about xenical or alternatives.
Cost, Accessibility, and Insurance Coverage Comparisons
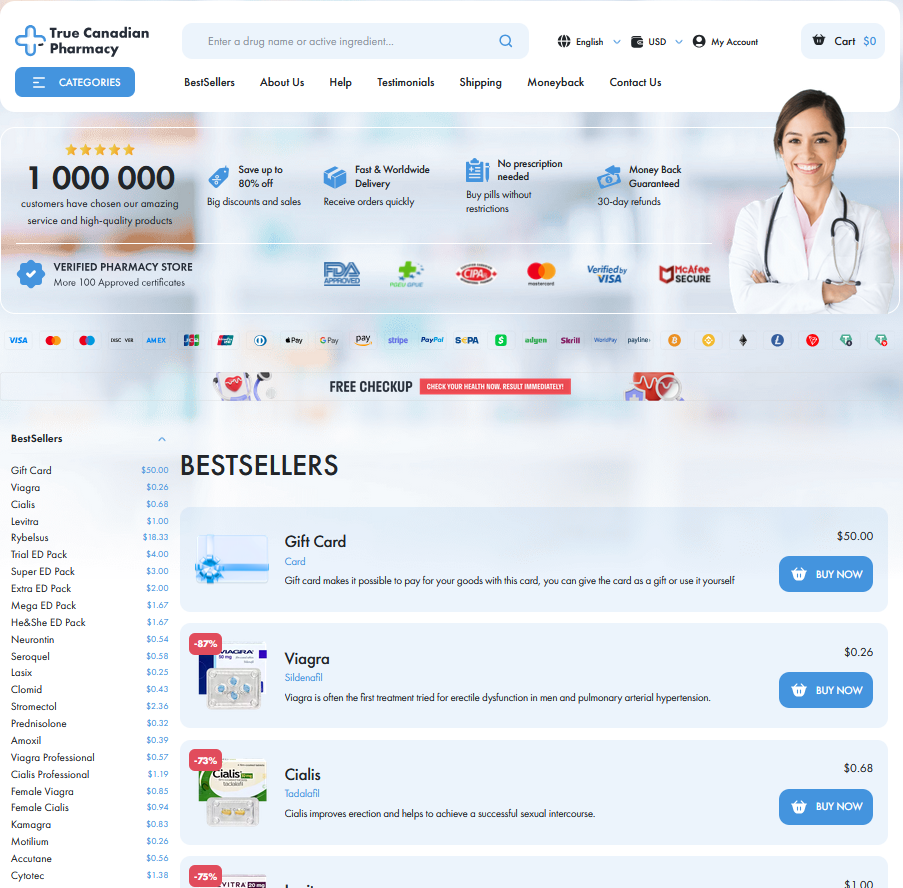
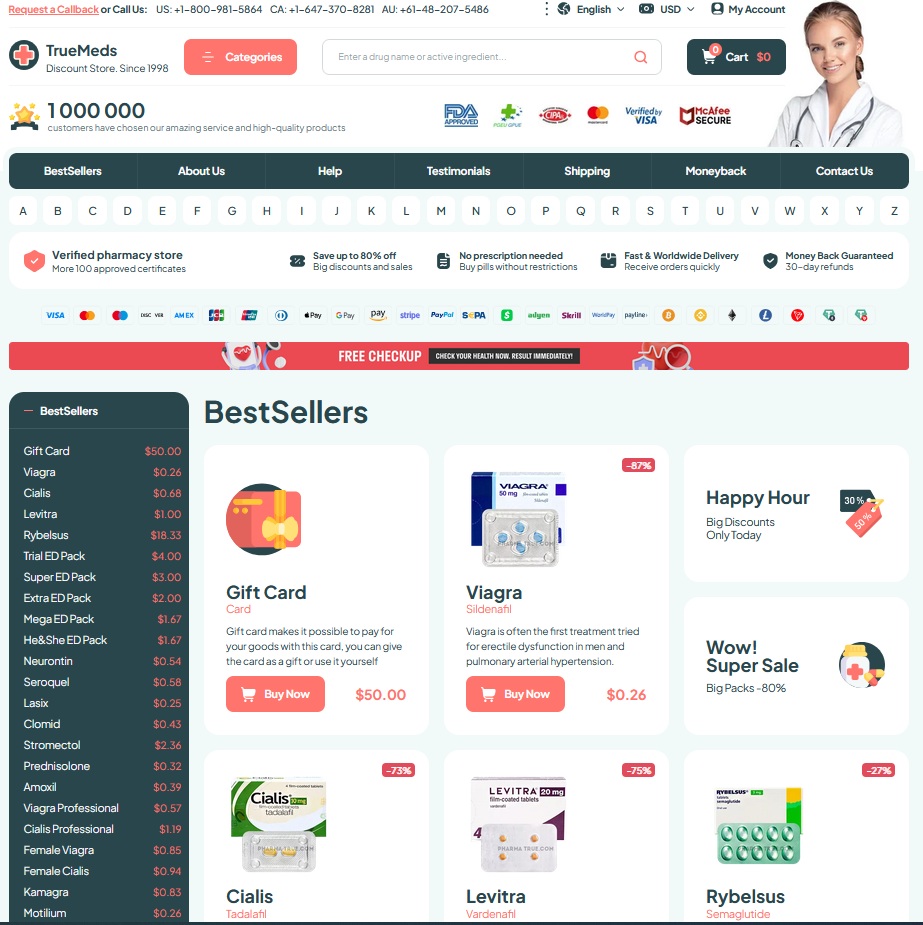
A practical shopper's perspective: xenical often feels pricier than generic alternatives, and retail pricing varies widely between pharmacies and online suppliers. Clinics and telehealth services sometimes offer bulk discounts, and community health programs can reduce upfront costs.
Insurance coverage can be a maze; some plans cover prescriptive weight drugs, others exclude them, and patients often need prior authorizations or step therapy that delay starts. Compare copays, deductibles, and manufacturer assistance for realistic budgeting.
Out-of-pocket burden leads patients to seek coupons; Occassionally they aquire cards or switch meds to lower costs.
Choosing the Right Medication: Patient Profiles and Outcomes
Picking a medication feels personal: one woman with insulin resistance chose orlistat because it works in the gut and avoids systemic effects, while a man with cardiovascular disease preferred a GLP-1 agonist for appetite suppression and metabolic benefit. Clinicians weigh comorbidities, pregnancy plans, and a patient’s willingness to change diet; they also consider how patients recieve counselling and follow-up. Age, prior attempts, and tolerability shape likely outcomes over time.
Outcomes depend on realistic expectations—modest average weight loss, variable side effects, and the need for behavioural support—so shared decision-making is essential. If GI intolerance or drug interactions occur, alternatives may be safer; if diabetes control is paramount, incretin therapies often deliver greater glycemic and weight improvements. Real-world adherence and lifestyle support strongly influence long-term success rates significantly. Discuss monitoring, duration, and cost with your clinician. NHS: Orlistat MedlinePlus: Orlistat